Children’s Vaccination
Immunisation is one of the most significant public health intervention in the last 200 years, providing a safe and efficient way to prevent the spread of many diseases that cause hospitalisation, serious ongoing health conditions and sometimes death.
Since the introduction of vaccination for children in Australia in 1932, deaths from vaccine-preventable diseases have fallen by 99 per cent, despite a threefold increase in the Australian population over that period. Worldwide, it has been estimated that immunisation programmes prevent approximately three million deaths each year.
Immunisation is critical for the health of children and the wider community. For immunisation to provide the greatest benefit, a sufficient number of people need to be vaccinated to halt the spread of bacteria and viruses that cause disease - a phenomenon called ‘herd immunity’. The proportion of the population that has to be immune to interrupt disease transmission differs for each vaccine preventable disease, but is around 90 per cent for most diseases. For a highly infectious disease like measles, this is up to 95 per cent of the population. This emphasises the need to stay vigilant and ensure high coverage rates are achieved, not only at the national level, but also at the local level.
In Australia, immunisation coverage rates for children are high, with over 90 per cent of children fully immunised at one, two and five years of age. This high rate of immunisation helps to maintain community immunity, especially for those who are too young to be immunised or those that are not able to be immunised for medical reasons. Without herd immunity, rare diseases will become common again, causing more illness and deaths.
Please consult your doctor for the latest immunisation schedule for your child.
Hepatitis B Vaccine – Hepatitis B virus targets the liver and hepatitis B vaccine (HBV) can prevent your child from developing chronic liver disease or liver cancer in future. It is administered four times, the first dose is given within a short period after birth for all infants before hospital discharge; the subsequent injections are usually given at 2, 4 and 6 months of age.
Pneumococcal Vaccine – The Pneumococcal vaccine (PCV) offers protection against the infections such as meningitis, blood infections and pneumonia caused by pneumococcal bacteria. PCV immunisations are given as a series of three injections at ages of 2 months, 4 months and the last dose at 6-months.
Diphtheria, Tetanus and Acellular Pertussis Vaccine – Diphtheria, Tetanus and acellular Pertussis Vaccine (DTaP vaccine) is a combination vaccine against diphtheria, tetanus and pertussis (whooping cough). The DTaP is scheduled as a series of 5 injections at ages 2 months, 4 months, 6 months, at 18 months and the last dose at 4 years. After these initial shots, a booster dose of the vaccine must be administered between 12 and 13 years or to the older teens and adults those who have not received a booster with pertussis coverage. Booster doses of Td (tetanus and diphtheria) should be given every 10 years thereafter. Booster doses: Older children/adolescents: additional booster dose is recommended for adolescents between 11 and 13 years of age, due to waning of the antibody response following the booster dose recommended at 4 years of age. Adults: Vaccination with dTpa is recommended for any adult who wishes to reduce their likelihood of becoming ill with pertussis
Haemophilus Influenza Type B Vaccine – Haemophilus influenza type b (Hib) disease is a serious condition caused by haemophilus influenza type b bacteria. The Hib vaccine is given at ages 2 months, 4 months, 6 months and a booster dose is given at 12 months. It provides long-term protection from Haemophilus influenza type b infections.
Poliovirus Vaccine – Inactivated poliovirus vaccine (IPV) is administered to protect your child from polio. Poliomyelitis or polio is a disease caused by polioviruses that can damage the nervous system, cause paralysis and can lead to death. Poliovirus vaccine is usually given at four doses at age 2 months, 4 months, 6 months and at 4 years.
Measles, Mumps and Rubella vaccine – The measles, mumps, and rubella (MMR) vaccine protects against measles, mumps and rubella. The MMR vaccines are injected as two doses, the first dose at 12 months and the second dose at 18 months.
Varicella Vaccine – Varicella vaccine protects against chicken pox, one of the common and a highly contagious childhood viral disease. The vaccine is recommended in children at 18 months.
Meningococcal Conjugate Vaccine – The meningococcal conjugate vaccine (MenCCV) is a vaccine used to protect infants and young children against meningococcal C disease, a bacterial infection caused by meningococcal bacteria. It is usually given at the age of 12 months.
Rotavirus Vaccine – Rotavirus is the leading cause of diarrhoea among infants and young children. The vaccine which is a liquid given by mouth in a two dose regime, first dose at between 6 and 8 weeks old and second dose at 4 months.
Human Papilloma Virus Vaccine- – Human papilloma virus (HPV) infection is the most common sexually transmitted infection that causes genital warts and precancerous changes in the uterine cervix leading to cervical cancer. The vaccine is recommended in a three dose schedule over a 6-month period; the vaccine is recommended between 12 and 13 years and also in older children who were not vaccinated before. This is generally provided as part of the school vaccination programme.
Side effects
Some vaccines may cause mild temporary side effects such as fever and soreness or swelling and redness at the site of injection. Serious reactions are rare and if any serious reactions are observed consult your doctor immediately. Your doctor/nurse may discuss with you all the possible risks and benefits of immunisation.
NSW School Vaccination Program 2019
NSW Health works in partnership with schools to offer the vaccines recommended for adolescents by the National Health and Medical Research Council (NHMRC) in a school-based vaccination program.
Parent information kits are sent home to parents early in the school year. To consent to vaccination, parents are advised to read all the information provided, complete and sign the consent form and return it to their child's school.
Students in high schools in 2019 will be offered the following vaccines:
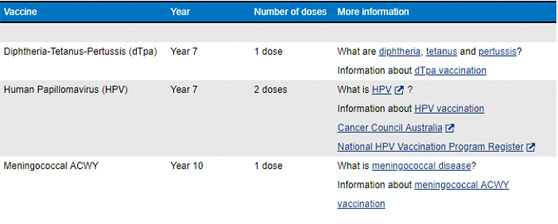
- Free vaccine is only available at school to students who have a signed consent form and who commence the vaccine course while they are in Year 7 (for dTpa or HPV vaccination) or Year 10 (for meningococcal ACWY vaccination).
- Students who miss vaccine doses due to absence on the day of the nurses' visit will be offered catch-up vaccination at subsequent school clinics. Where this is not possible, parents will be advised that free catch-up vaccine is available at their local GP.
- Parents who choose to wait for their child to be older before consenting to vaccination will be required to arrange for vaccination at their GP and may have to pay a consultation fee. More information is available about catch-up vaccination .
- Parents can withdraw consent at any time before vaccination takes place.
- Coverage rates for all vaccines offered to students in high schools from 2011 to 2017 are available.
- Information about the vaccinations is also available in 26 community languages .
- A video (Whatchya Gunna DO?) has been produced to raise awareness about the importance of immunisation for Aboriginal adolescents and their parents.
The NSW Immunisation schedule (as of 1 July 2018):
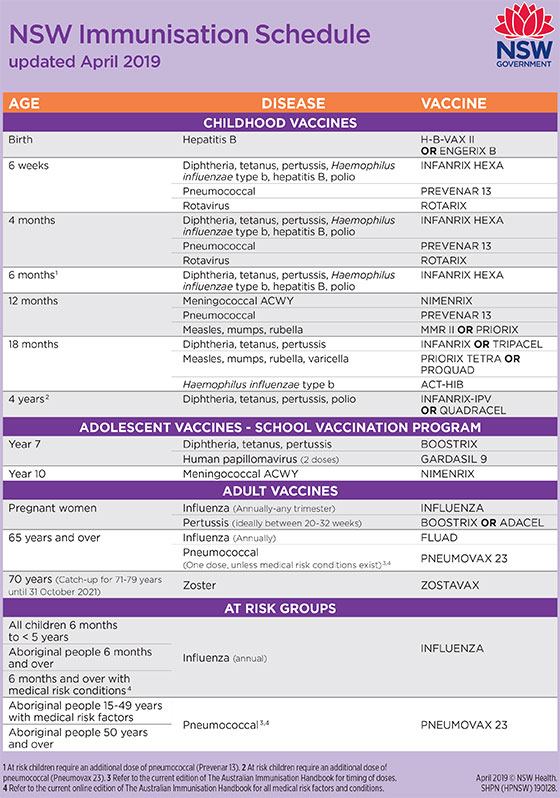
Alternatively, please click the link to access the NSW Immunisation schedule as of April 2019: NSW Immunisation schedule




